A new study led by Sam Chakrabarti investigates the role of lubricating fluid in pain associated with osteoarthritis.
I want my research to contribute towards a world where pain relief is safe and affordable, a world where the reason people take time off work is to go on vacation, not because they are in excruciating pain.
Sam Chakrabarti
A research study led by a Gates Cambridge Scholar has shown how, in osteoarthritis patients, the viscous lubricant that ordinarily allows our joints to move smoothly triggers a pain response from nerve cells similar that caused by chilli peppers.
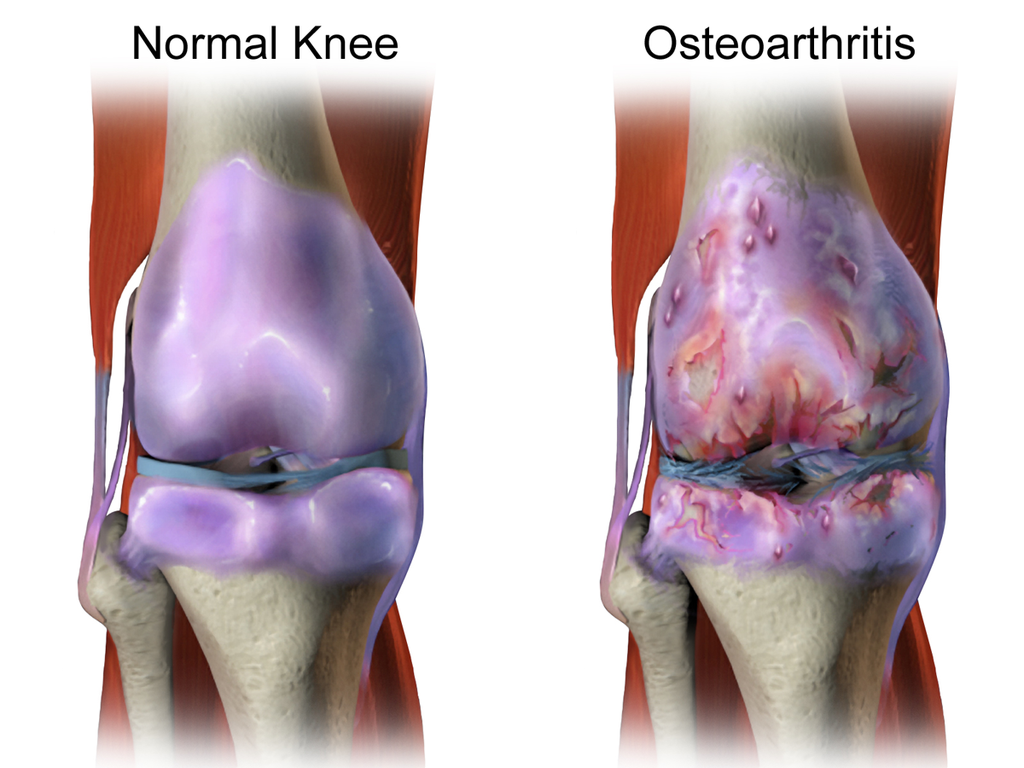
Osteoarthritis is the most common form of arthritis. It causes joint pain and stiffness, and in some people swelling and tenderness of the joints. The condition affects an individual’s quality of life and costs millions to the global economy, both directly in terms of healthcare costs and indirectly due to impact on the individual’s working life.
Osteoarthritis tends to occur later in life and has been largely considered as a degenerative disorder in which pain is produced by damage and wear and tear to bone and cartilage. However, in recent years it has become clear that osteoarthritis is not restricted to cartilage damage, but is a failure of the entire joint, with inflammation – the body’s response to stress and injury – being a major contributor to the pain experienced by patients. A recent collaboration between the two pharmaceutical companies Pfizer and Eli Lilly has found that their anti-inflammatory drug, tanezumab, produced pain relief for osteoarthritic patients in a phase 3 clinical trial.
When inflammation occurs during osteoarthritis, the body produces an increased number of cells within and around the joint. These cells release inflammatory substances into the synovial fluid, the lubricant that allows joints to move smoothly. During osteoarthritis, synovial fluid becomes less viscous and these inflammatory substances come into direct contact with sensory nerve cells in the joint, producing the sensation of pain.
In a study published on 13 August 2019 in the journal Rheumatology, researchers at the University of Cambridge and Addenbrooke’s Hospital, part of Cambridge University Hospitals, examined whether synovial fluid produced during osteoarthritis is capable of directly exciting sensory nerves supplying knee joints – those nerves responsible for transmitting pain signals.
“Osteoarthritis can be a very painful condition, but we only know a little about what causes this pain,” says Gates Cambridge Scholar Sam Chakrabarti [2016] who is doing a PhD in Pharmacology. “We wanted to investigate what was happening in the joint and to see whether it was the lubricant that ordinarily keeps these joints moving that was contributing to the pain. Studies such as these are important in helping us develop better treatments.”
The researchers obtained synovial fluid from consenting osteoarthritis patients at Addenbrooke’s Hospital and from post-mortem donors with no known joint disease. They then incubated knee sensory nerves isolated from mice in either healthy or osteoarthritis synovial fluid and recorded the activity of these nerves.
The team found that when incubated with osteoarthritic synovial fluid, the knee nerves were more excitable. The nerves also showed an increase in the function of TRPV1, a molecule that detects the hotness of chilli peppers (TRPV1 is also activated by heat, which is why chillis tastes hot). Although the presence of inflammatory chemicals in osteoarthritis synovial fluid has been known since 1959, this is the first evidence that synovial fluid can directly excite sensory nerves and hence is an important contributor to an individual’s experience of pain.
“This is the first time we have been able to use synovial fluid from human osteoarthritis patients to excite sensory nerve cells, making it more clinically-relevant than mouse studies alone, and so will hopefully help translating treatments from bench to bedside,” says Dr Ewan St John Smith from the Department of Pharmacology at the University of Cambridge.
“In the future, this set up can be used to identify the specific components of synovial fluid that cause pain and then to test if and how a drug will be useful in arthritic pain. Since synovial fluid is regularly collected from arthritic patients as part of their treatment regime, our technique can be easily set up in laboratories throughout the world to understand and help to identify a cure for arthritic pain.”
Dr Deepak Jadon, Director of the Rheumatology Research Unit at Cambridge University Hospitals, adds: “This study highlights how much we can learn with the help of our patients, as well as the importance of collaboration between clinicians and basic scientists.”
Sam says: “I want my research to contribute towards a world where pain relief is safe and affordable, a world where the reason people take time off work is to go on vacation, not because they are in excruciating pain."
Originally from Kolkata, India, she is interested in finding better ways of studying painful knee arthritis to help identify drug targets. Arthritis affects millions of people worldwide, but patients often receive inadequate pain relief. A major reason for this is the lack of understanding of the basic biology underlying the disease, but Sam recognises that tackling arthritic pain will require a much broader approach than basic science.
“I hope my research will lead to an understanding of pain that crosses many disciplines and breaks down the language barrier between psychologists, biologists and computer scientists,” she says. “Pain is complex and manifests at multiple levels – a way to understand a phenomenon like this should also be multidisciplinary.”
*The research was funded by Versus Arthritis and the Gates Cambridge Trust. Picture credit: Courtesy of Bruce Blaus and Wikimedia commons.
Sampurna Chakrabarti
- Alumni
- India
- 2016 PhD Pharmacology
- Corpus Christi College
Originally from India, I graduated in May 2016 with B.S. in Biological Sciences and B.A. in Psychology from The State University of New York at Buffalo, USA. For my PhD, I studied mechanisms of inflammatory knee pain in the lab of Dr. Ewan St. John Smith at the Department of Pharmacology. Currently I am a Alexander von Humboldt fellow researching how we perceive touch at the Max Delbrueck Center for Molecular Medicine in Berlin, Germany. I am also passionate about educational equality and hope to work with organizations around the world, especially in developing countries, to make quality education available to all. I am honoured and excited to become a member of the vibrant and compassionate Gates Cambridge community where scholars from across the world share the vision of making a difference in the world.
Previous Education
University at Buffalo












